Piriformis Syndrome often goes unnoticed until the discomfort becomes too intense to ignore. It usually starts with a subtle pain in the buttock region that gradually radiates down the back of the leg, sometimes mimicking sciatica. Recognizing the signs early and understanding the underlying causes is crucial for timely management.
As a physiotherapist, I have encountered many individuals who struggle with Piriformis Syndrome and its impact on daily mobility. Addressing this condition effectively involves a thorough assessment, targeted interventions, and awareness of preventive strategies that can significantly reduce discomfort and improve overall quality of life.
What Is Piriformis Syndrome?
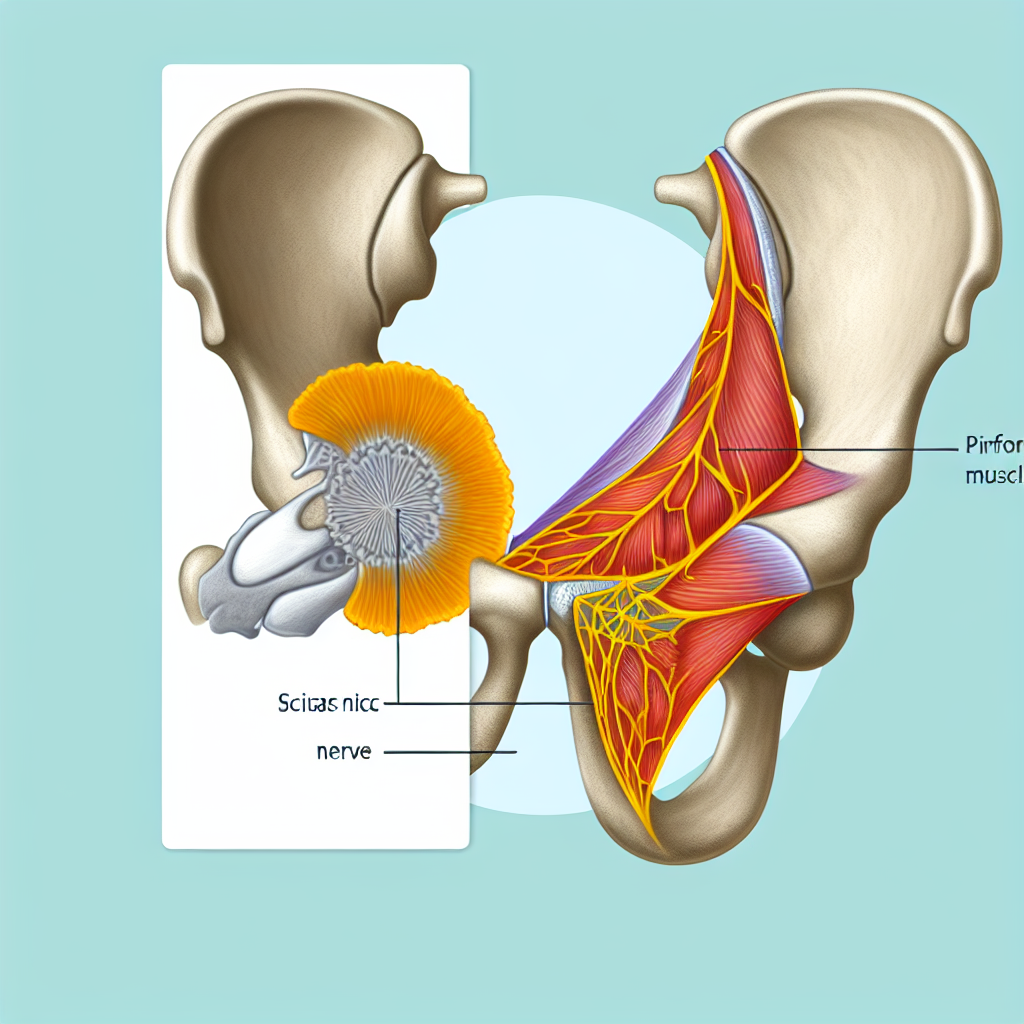
Piriformis Syndrome is a neuromuscular condition that occurs when the piriformis muscle, located in the buttock region, irritates or compresses the sciatic nerve. This often leads to pain, tingling, and numbness that may travel down the back of the leg. Although it closely resembles sciatica, which is primarily caused by spinal nerve root compression, Piriformis Syndrome specifically stems from issues related to the piriformis muscle itself.
In many cases, Piriformis Syndrome can be challenging to diagnose because its symptoms overlap with other conditions that affect the lower back and hips. However, proper clinical assessment and an understanding of the piriformis muscle’s role can help differentiate it from other causes of sciatic nerve pain. By pinpointing the culprit as the piriformis muscle, targeted interventions can be employed to alleviate the nerve irritation and restore pain-free movement.
Anatomy of the Piriformis Syndrome
The piriformis muscle is a small, flat band of muscle that stretches from the sacrum (the triangular bone at the base of the spine) to the top of the femur (thigh bone). Despite its modest size, the piriformis plays a significant role in lower-limb function:
- Hip External Rotation: The piriformis muscle helps rotate the thigh outward.
- Stabilization of the Hip Joint: It contributes to hip stability, especially during walking and running.
- Proximity to the Sciatic Nerve: The piriformis muscle lies just over the sciatic nerve, which is the largest nerve in the human body. Any inflammation or tightness in the piriformis muscle can impact this crucial nerve.
Because of its close relationship to the sciatic nerve, dysfunction in the piriformis muscle can create considerable discomfort and nerve-related issues. In some individuals, the sciatic nerve may even pass through the piriformis muscle fibers, increasing the likelihood of entrapment and subsequent development of Piriformis Syndrome.
What causes Piriformis Syndrome?
Multiple factors can lead to Piriformis Syndrome. Identifying the primary cause is essential for proper treatment and prevention of recurrence. These are some common causes and contributing factors:
- Overuse or Repetitive Stress
Activities involving excessive hip rotation or prolonged sitting can strain the piriformis.
Sports like tennis, rowing, or running can place repeated stress on the buttock region.
- Muscle Imbalances
Weakness or tightness in surrounding muscles (e.g., glutes, hip flexors) can force the piriformis to overcompensate.
Pelvic misalignment may alter the mechanics of the hip, increasing stress on the piriformis muscle.
- Trauma or Injury
Direct impact to the buttock or hip, such as a fall or collision, can injure the piriformis.
Scar tissue formation from previous injuries can disrupt muscle function.
- Poor Posture and Prolonged Sitting
Sitting for extended periods can compress the piriformis muscle and the sciatic nerve beneath it.
Slouching postures that tilt the pelvis can put additional stress on the lower back and hips.
- Biological Variations
Anatomical differences, like a split piriformis or nerve anomalies, can predispose a person to Piriformis Syndrome.
Pinpointing the exact cause of Piriformis Syndrome allows for a targeted rehabilitation approach. Even everyday activities can trigger or worsen this condition, so understanding these factors helps tailor preventive strategies and interventions.
What are the Symptoms of Piriformis Syndrome?
Piriformis Syndrome can present with a wide range of symptoms, many of which mirror other conditions affecting the sciatic nerve. Recognizing these specific features can lead to a more accurate diagnosis:
- Buttock Pain
A deep, aching discomfort felt in the buttock area is often the earliest sign.
Pain can increase when sitting on hard surfaces or after prolonged periods of inactivity.
- Referred Pain in the Leg
The discomfort may travel down the back of the thigh and sometimes into the calf.
It can be described as sharp, shooting, or tingling, resembling classic sciatica.
- Numbness or Tingling
Some individuals report a sensation of pins and needles radiating from the buttock down the leg.
- Difficulty Sitting or Walking
Extended sitting often aggravates the pain due to increased pressure on the piriformis and sciatic nerve.
Walking or climbing stairs may be challenging if the piriformis is inflamed or in spasm.
- Pain with Hip Movements
Simple actions such as rotating the hip outward or crossing the legs may intensify symptoms.
- Reduced Range of Motion
The inflamed or tight piriformis muscle may limit hip mobility and flexibility.
Because these symptoms overlap with other possible diagnoses (like lumbar spine pathologies), a thorough clinical evaluation is crucial. Identifying whether the pain originates from the piriformis muscle specifically will guide physiotherapists and other healthcare professionals in implementing the most effective treatment strategies.
Special test of Piriformis Syndrome
Evaluating Piriformis Syndrome involves certain clinical tests designed to provoke the pain or isolate the muscle’s function. These special tests help practitioners discern whether the piriformis muscle is causing sciatic nerve compression. Below is a list of commonly used physical examination maneuvers, along with explanations on how they are performed.
FAIR Test (Flexion, Adduction, and Internal Rotation)
- Position: The patient lies on the unaffected side (side without pain).
- Movement: The examiner flexes the hip and knee of the painful side and then moves the hip into adduction and internal rotation.
- Positive Sign: Reproduction or worsening of buttock pain or sciatica-like symptoms indicates possible Piriformis Syndrome.
Pace’s Test
- Position: The patient sits on the edge of the examination table with knees bent at 90 degrees, feet on the floor.
- Movement: The examiner places their hands on the patient’s knees and asks the patient to abduct and externally rotate the hips against resistance.
- Positive Sign: Pain or weakness during this resisted movement suggests piriformis involvement.
Freiberg’s Sign
- Position: The patient lies supine (face up) on the table.
- Movement: The examiner passively moves the affected hip into forced internal rotation.
- Positive Sign: Sharp pain in the buttock region that may radiate down the leg can indicate Piriformis Syndrome.
Beatty’s Maneuver
- Position: The patient lies on the back with knees bent.
- Movement: The patient actively lifts the symptomatic leg, placing the foot on the opposite knee to create a figure-4 shape.
- Positive Sign: Buttock or leg pain that emerges or worsens in this position is suggestive of piriformis-related sciatic nerve irritation.
Seated Piriformis Stretch Test
- Position: The patient sits with feet flat on the floor.
- Movement: The patient places the ankle of the affected side over the opposite knee and slowly leans forward.
- Positive Sign: Increased pain or tingling in the buttock and leg indicates possible compression of the sciatic nerve by the piriformis muscle.
Summary Table of Special Tests
| Test Name | Patient Position | Examiner Action | Positive Sign |
|---|---|---|---|
| FAIR Test | Side-lying, painful side up | Flex, adduct, internally rotate the hip | Buttock/leg pain |
| Pace’s Test | Seated | Resisted abduction & external rotation of hips | Pain or weakness |
| Freiberg’s Sign | Supine | Passive forced internal rotation of the hip | Buttock/leg pain |
| Beatty’s Maneuver | Supine, hips flexed | Patient crosses foot over opposite knee, forming figure-4 | Buttock/leg pain |
| Seated Piriformis Stretch | Seated | Patient crosses ankle over knee & leans forward | Buttock/leg pain |
These tests, used together with a patient’s history and clinical findings, can strongly suggest Piriformis Syndrome if they provoke symptoms. However, confirming this condition often involves ruling out lumbar spine pathologies or other hip-related issues.
How do we Treat Piriformis Syndrome
Managing Piriformis Syndrome effectively typically involves a combination of therapeutic exercises, manual techniques, and lifestyle modifications. By addressing factors that led to the development of this condition, patients experience relief and reduce the likelihood of recurrence. Treatment aims to:
- Decrease inflammation and pain in the piriformis muscle.
- Alleviate pressure on the sciatic nerve.
- Restore normal movement and function.
- Correct muscular imbalances and poor biomechanical patterns.
Below are several approaches frequently employed to treat Piriformis Syndrome.
Piriformis Syndrome Treatment Approaches
Physiotherapy Exercises
Gentle Stretches: Target the piriformis, gluteal muscles, and surrounding structures to improve flexibility.
Strengthening Routines: Strengthen the hip abductors, external rotators, and core muscles to enhance pelvic stability.
Gradual Progression: Exercise intensity should increase step by step to prevent re-injury.
Manual Therapy Techniques
Soft Tissue Mobilization: Helps reduce muscle tension and break down adhesions.
Myofascial Release: Targets tight fascial structures around the piriformis muscle.
Trigger Point Therapy: Addresses knots or areas of hyperirritability within the muscle that can cause radiating pain.
Electrophysical Modalities
Ultrasound Therapy: May help with blood flow enhancement and tissue healing.
Transcutaneous Electrical Nerve Stimulation (TENS): Aims to alleviate pain by modulating nerve signals.
Heat and Cold Therapy
Ice Packs: Applied immediately after activity to reduce inflammation.
Heat Packs: Used before stretching or exercise to relax the muscle tissue and improve blood flow.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Used under medical supervision to decrease pain and inflammation.
Lifestyle Modifications
Ergonomic Adjustments: Encouraging proper posture and supportive seating to reduce pressure on the piriformis muscle.
Activity Modification: Guiding patients to balance rest and movement, and to avoid repetitive stress on the hip.
Weight Management: Maintaining a healthy weight helps limit undue pressure on the lower back and hips.
Dry Needling or Acupuncture
Targets trigger points in the piriformis muscle to relax tight fibers and reduce pain transmission.
Corticosteroid Injections
A specialized medical intervention for cases that do not respond to conservative management.
Helps reduce inflammation in and around the piriformis muscle.
Surgical Intervention
Considered only in rare and severe cases where nerve compression cannot be alleviated through conservative means.
Combining these treatments in a comprehensive management plan can yield the best outcome for individuals experiencing Piriformis Syndrome. A tailored approach, guided by a physiotherapist, ensures each intervention targets the patient’s unique presentation.
Piriformis Syndrome Differential Diagnosis
Because Piriformis Syndrome closely resembles other conditions that cause sciatic nerve pain, ruling out alternative diagnoses is important. This process allows healthcare professionals to tailor therapies accurately. Here are some key differential diagnoses:
Lumbar Disc Herniation
Herniated discs in the lower back may compress the sciatic nerve, leading to similar pain patterns.
Assessment often includes imaging (MRI) and neurological tests to identify nerve root compression.
Spinal Stenosis
Narrowing of the spinal canal can trap nerve roots, causing pain, numbness, or weakness in the legs.
Older adults and individuals with degenerative changes in the spine are more prone to stenosis.
Dysfunction in the sacroiliac joint (SIJ) can mimic sciatic nerve pain by referring discomfort to the buttock and thigh.
Specific SIJ tests and imaging can help differentiate from Piriformis Syndrome.
Hamstring Injuries
Strains or tendon issues in the hamstrings may cause deep buttock and posterior thigh pain.
Provocative tests focusing on hamstring tension can help distinguish the origin of pain.
Gluteal Tendinopathy
Overload or degenerative changes in the gluteal tendons can present with lateral hip or buttock pain.
Specific resisted abduction tests often clarify if the piriformis or gluteal tendons are implicated.
Sciatic Nerve Tumors or Cysts
Rare, but possible, growths along the sciatic nerve pathway can cause symptoms similar to Piriformis Syndrome.
Imaging such as MRI can detect these anomalies.
Differentiating these conditions typically involves a detailed patient history, physical examinations, and sometimes imaging studies. Correctly identifying Piriformis Syndrome ensures that treatments target the true source of discomfort rather than merely alleviating symptoms.
Piriformis Syndrome Prognosis and Expectations
Individuals experiencing Piriformis Syndrome often regain their pain-free mobility through the correct application of conservative treatments. While prognosis can vary based on factors like injury severity, duration of symptoms, and patient compliance with rehabilitation, most people observe significant improvement within a few weeks to a few months. Key considerations for long-term success include:
Consistent Rehabilitation
Adhering to physiotherapy exercises and stretching routines fosters muscle balance and prevents re-injury.
Activity Modification
Adjusting daily activities, sports training, or exercise routines can avert future flare-ups.
Incorporating regular breaks and ergonomic aids reduces prolonged strain on the buttock and hip area.
Maintenance Exercises
Continuing low-level strengthening and flexibility exercises helps preserve hip stability and piriformis muscle health.
Patients often benefit from adding cross-training and core-focused workouts to their weekly regimen.
Awareness of Posture and Body Mechanics
Maintaining proper posture during standing, sitting, and lifting prevents repetitive stress on the piriformis.
Small adjustments, such as using a lumbar roll or an ergonomic chair, can lessen sciatic nerve compression.
Healthy Lifestyle Choices
Keeping body weight within a healthy range lessens stress on the lower body.
Balanced nutrition supports muscle recovery and helps maintain overall health.
Staying hydrated can also aid in muscle and nerve function.
In many instances, individuals fully recover and return to their usual activities without limitations once Piriformis Syndrome resolves. However, occasional monitoring or refresher physiotherapy sessions may be advised to ensure no recurrence or compensatory issues develop.
Closing Thoughts
Piriformis Syndrome can be an unsettling experience, primarily because it often mirrors other more well-known conditions like sciatica. By comprehensively examining the symptoms, understanding the anatomy of the piriformis muscle, and using specialized physical tests, healthcare professionals can accurately pinpoint this condition. Treatment focuses on reducing muscle tension, minimizing sciatic nerve compression, and teaching patients strategies to prevent recurrences.
As a physiotherapist, I emphasize a tailored approach that respects each person’s unique posture, muscle imbalances, and activity levels. Consistent adherence to physiotherapy exercises, combined with proactive lifestyle modifications, enhances results and paves the way for a full recovery from Piriformis Syndrome. Whether it manifests from prolonged sitting, intense athletic pursuits, or muscular imbalances, timely intervention, and proper self-care can alleviate pain and restore day-to-day comfort and function.
