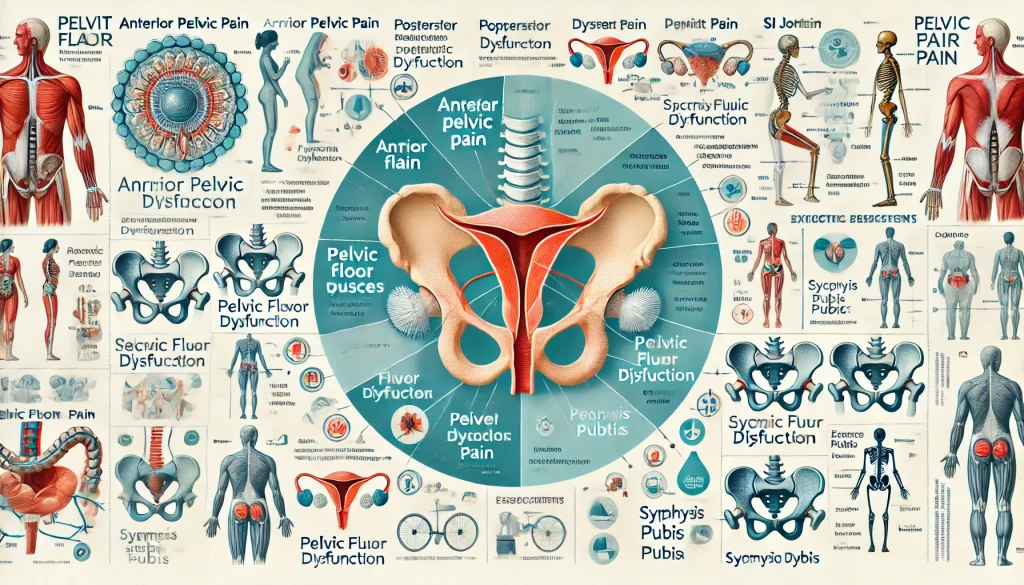
Pelvic pain is a complex and often debilitating condition that can affect individuals across all stages of life. The pelvis, which is a central part of the body’s structure, contains several organs, muscles, ligaments, and nerves that can be sources of discomfort.
While pelvic pain is commonly associated with pregnancy or childbirth, it can arise from a wide range of conditions that affect both men and women.
Whether the pain is acute or chronic, localized or radiating, understanding the different types and causes of pelvic pain can be key to effectively managing and treating it.
This comprehensive article will cover the various types of pelvic pain, specific conditions that contribute to discomfort, gender-specific issues, and the impact of pelvic pain on overall well-being.
Types of Pelvic Pain
Pelvic pain can present in different locations within the pelvic region, each with distinct causes and symptoms. Identifying the type of pelvic pain is crucial for accurate diagnosis and treatment.
1. Anterior Pelvic Pain
Anterior pelvic pain refers to pain that is felt in the front part of the pelvis, often in the lower abdomen or groin area. This type of pain can be sharp, dull, or aching and may radiate to the hips or thighs.
Causes:
- Pelvic Organ Disorders: Conditions affecting the bladder, uterus, or ovaries, such as cysts or endometriosis, can cause anterior pelvic pain.
- Hernia: Inguinal hernias or femoral hernias can manifest as pain in the lower abdomen and groin.
- Pelvic Muscle Strain: Overuse of the pelvic muscles, such as from heavy lifting or intense physical activity, can lead to anterior pelvic pain.
Symptoms:
- Pain in the lower abdomen, groin, or front of the pelvis.
- Pain may worsen with certain movements, such as bending or lifting.
- Often associated with urinary or gastrointestinal issues.
Management: Treatment often involves physical therapy, medication for pain relief, addressing any underlying conditions (such as pelvic organ issues), and modifications to activity levels.
2. Posterior Pelvic Pain
Posterior pelvic pain occurs in the lower back, sacrum, and buttocks region. This type of pain can be chronic and often leads to discomfort during movement, such as sitting, standing, or walking.
Causes:
- Sacroiliac (SI) Joint Dysfunction: Dysfunction of the SI joint, which connects the sacrum to the pelvis, is a common cause of posterior pelvic pain.
- Muscle Strain: Overuse or injury to the muscles of the lower back and buttocks can result in posterior pelvic pain.
- Pelvic Floor Dysfunction: Dysfunction in the pelvic floor muscles can contribute to pain that radiates to the lower back.
Symptoms:
- Dull or sharp pain in the lower back, sacrum, or buttocks.
- Pain may radiate down the legs or increase with activity.
- Difficulty with mobility, particularly when standing or sitting for extended periods.
Management: Treatments may include physical therapy focused on strengthening and stabilizing the pelvic floor, manual therapy for the SI joint, and lifestyle modifications to alleviate strain on the lower back.
3. Pelvic Floor Dysfunction
Pelvic floor dysfunction occurs when the muscles of the pelvic floor (which support the organs in the pelvis) become weakened, tight, or dysfunctional. This can lead to pain, discomfort, and difficulties with organ function.
Causes:
- Childbirth: Trauma to the pelvic floor muscles during labor and delivery can lead to dysfunction.
- Chronic Straining: Constipation, heavy lifting, and chronic coughing can strain the pelvic floor muscles.
- Aging: As people age, the pelvic floor muscles can weaken, leading to dysfunction.
Symptoms:
- Painful intercourse (dyspareunia).
- Urinary incontinence or urgency.
- Chronic pelvic pain or pressure in the lower abdomen or pelvis.
Management: Treatment may involve pelvic floor physical therapy, biofeedback, strengthening exercises, and in some cases, surgical interventions for severe dysfunction.
4. Sacroiliac (SI) Joint Pain
SI joint pain occurs when there is dysfunction in the sacroiliac joint, which connects the sacrum (lower spine) to the ilium (part of the pelvis). This type of pain is typically felt in the lower back or buttocks.
Causes:
- Joint Dysfunction: Arthritis, injury, or abnormal movement patterns can cause the SI joint to become misaligned or inflamed.
- Pregnancy: Hormonal changes and the added weight of pregnancy can lead to SI joint instability.
Symptoms:
- Deep, aching pain in the lower back or buttocks, sometimes radiating to the thighs.
- Pain worsens with standing, walking, or changing positions.
- Limited range of motion in the lower back and pelvis.
Management: Physical therapy, SI joint injections, chiropractic care, and in some cases, surgical stabilization of the joint can help alleviate symptoms.
Specific Conditions Related to Pelvic Pain
Certain specific conditions, particularly those related to pregnancy, childbirth, and physical strain, contribute to the development of pelvic pain. Understanding these conditions is essential for managing symptoms and improving quality of life.
1. Pregnancy-Related Pain
Pregnancy-related pelvic pain is common, especially in the second and third trimesters. The body undergoes numerous changes, including hormonal shifts and physical strain, which can lead to discomfort.
Causes:
- Hormonal Changes: Increased levels of relaxin during pregnancy cause the ligaments and muscles of the pelvis to loosen, leading to instability and pain.
- Growing Uterus: As the baby grows, it puts additional pressure on the pelvic region, contributing to discomfort.
- Pelvic Girdle Pain: This term refers to pain in the pelvic region caused by joint instability, particularly in the sacroiliac joint or symphysis pubis.
Symptoms:
- Aching or sharp pain in the lower abdomen, groin, or lower back.
- Difficulty walking, climbing stairs, or getting in and out of bed.
- Pain that worsens with prolonged standing, walking, or certain movements.
Management: Treatment includes pelvic floor exercises, using a maternity support belt, heat or cold therapy, and lifestyle adjustments to reduce strain.
2. Postpartum Pelvic Pain
Postpartum pelvic pain occurs after childbirth and is often related to the trauma of labor and delivery. The pelvic muscles, ligaments, and joints may take time to return to their pre-pregnancy state, leading to pain and discomfort.
Causes:
- Pelvic Floor Weakness: The pelvic floor muscles can be stretched or weakened during labor, contributing to pain and dysfunction.
- SI Joint Dysfunction: Pregnancy-related SI joint instability can persist postpartum.
- Abdominal Separation (Diastasis Recti): The separation of the abdominal muscles during pregnancy can strain the pelvic region.
Symptoms:
- Pain in the lower abdomen, pelvis, or perineum.
- Difficulty with physical activities such as lifting, walking, or bending.
- Pelvic floor issues like incontinence or painful intercourse.
Management: Physical therapy to strengthen the pelvic floor and core muscles, along with addressing any joint instability, is key to recovery.
3. Athletic Pubalgia (Sports Hernia)
Athletic pubalgia, often referred to as a sports hernia, is a condition characterized by chronic groin pain, which can be aggravated by physical activity.
Causes:
- Overuse of the Groin Muscles: Repetitive sports movements, particularly in sports that require sudden twisting or turning (e.g., football, soccer), can strain the muscles of the lower abdomen and groin.
- Tear in the Pubic Ligament: The condition often involves a tear or strain of the muscles and ligaments surrounding the pubic area.
Symptoms:
- Pain in the groin area, particularly during athletic activity.
- Discomfort when twisting, turning, or kicking.
- Pain that improves with rest but returns with activity.
Management: Treatment typically involves rest, ice therapy, physical therapy, and in some cases, surgery to repair the torn tissue.
4. Symphysis Pubis Dysfunction (SPD)
SPD occurs when the pubic symphysis, the joint at the front of the pelvis, becomes unstable or misaligned. This condition is most common during pregnancy but can also occur in non-pregnant individuals.
Causes:
- Hormonal Changes During Pregnancy: Relaxin hormone increases the mobility of the pubic symphysis in preparation for childbirth.
- Trauma or Injury: A fall or injury to the pelvis can lead to dysfunction of the pubic symphysis.
Symptoms:
- Pain in the pubic region, lower abdomen, or groin.
- Worsening pain with activities like walking, climbing stairs, or turning over in bed.
- A feeling of instability or “clicking” in the pelvis.
Management: Physical therapy, pelvic support belts, and modifications to daily activities can help alleviate symptoms. In severe cases, medical intervention may be necessary.
5. Coccydynia
Coccydynia refers to pain in the coccyx (tailbone) area, which is located at the bottom of the spine. This condition can be caused by trauma or prolonged sitting on hard surfaces.
Causes:
- Trauma: A fall onto the tailbone can cause bruising or injury.
- Prolonged Sitting: Sitting for long periods, particularly on hard or uncomfortable surfaces, can irritate the cocyx.
- Childbirth: During delivery, pressure on the tailbone can cause pain or injury.
Symptoms:
- Pain at the base of the spine, especially when sitting.
- Discomfort when standing up from a seated position.
- Tenderness or bruising around the tailbone area.
Management: Treatment includes using cushioned seating, applying heat or cold to the area, and avoiding prolonged sitting. In some cases, physical therapy or injections may be required.
6. Pelvic Floor Tension
Pelvic floor tension occurs when the muscles of the pelvic floor become excessively tight or overactive, leading to pain and dysfunction.
Causes:
- Chronic Stress: Emotional stress can cause the pelvic floor muscles to tighten.
- Trauma or Injury: Injury to the pelvic region can lead to muscle guarding.
- Childbirth: The trauma of labor can result in pelvic floor muscle dysfunction, leading to tension.
Symptoms:
- Pain during sexual intercourse.
- Difficulty with urination or bowel movements.
- Chronic pelvic pain or pressure.
Management: Treatment involves pelvic floor physical therapy to relax and strengthen the muscles, as well as mindfulness and relaxation techniques to reduce stress.
Gender-Specific Issues
Pelvic pain can manifest differently in men and women due to anatomical and physiological differences, as well as distinct health concerns related to gender.
1. Male Pelvic Pain
Male pelvic pain often involves issues with the prostate, bladder, or pelvic floor. Conditions such as prostatitis, pelvic floor dysfunction, or nerve entrapment can lead to persistent discomfort.
Causes:
- Prostatitis: Inflammation of the prostate gland can lead to pelvic pain.
- Pelvic Floor Dysfunction: Men can also experience pelvic floor tension or weakness, contributing to pain.
- Hernias: Inguinal hernias or other abdominal hernias can refer pain to the pelvic area.
Symptoms:
- Pain in the lower abdomen, perineum, or groin.
- Discomfort or pain during urination or sexual activity.
- Chronic pain that worsens with sitting or standing for long periods.
Management: Treatment may involve physical therapy, medications for inflammation or pain, and in some cases, surgery to address any underlying issues like hernias or prostate problems.
2. Female Pelvic Pain
Female pelvic pain often involves reproductive organs such as the uterus, ovaries, and fallopian tubes. Conditions like endometriosis, fibroids, or pelvic inflammatory disease (PID) are common causes.
Causes:
- Endometriosis: Tissue similar to the uterine lining grows outside the uterus, causing pain.
- Fibroids: Non-cancerous growths in the uterus that can cause pain, especially during menstruation.
- Pelvic Inflammatory Disease: An infection of the reproductive organs that leads to pelvic discomfort.
Symptoms:
- Pain during menstruation, intercourse, or urination.
- Chronic lower abdominal or pelvic pain.
- Pain associated with bowel movements or urinary urgency.
Management: Treatment often involves medications for pain and inflammation, hormone therapy, or surgical options like a hysterectomy or laparoscopy for conditions like endometriosis.
3. Pregnancy Considerations
Overview: During pregnancy, the body undergoes numerous changes that can lead to pelvic pain. These changes include hormonal shifts, weight gain, and alterations in posture.
Causes:
- Hormonal Changes: Relaxin and other hormones cause ligaments and joints to become looser in preparation for childbirth, contributing to pelvic pain.
- Growing Uterus: The expanding uterus places pressure on the pelvic structures.
- Postural Changes: Weight gain and changes in the center of gravity can strain the pelvic muscles and ligaments.
Symptoms:
- Lower back pain, sacroiliac pain, or groin pain.
- Pelvic pressure or pain when walking or standing.
- Pain with changing positions or getting in and out of bed.
Management: Treatment includes pelvic support belts, physical therapy, gentle exercise, and modifications to daily activity to alleviate strain.
4. Post-Surgical Recovery
Pelvic pain following surgery, particularly pelvic or abdominal surgery, can be a common issue during the recovery period.
Causes:
- Scar Tissue (Adhesions): After surgery, scar tissue can form, leading to chronic pelvic pain.
- Nerve Damage: Nerve injury during surgery can result in persistent pain or numbness.
- Infection: Post-surgical infections can cause inflammation and pain.
Symptoms:
- Persistent pain at the site of the surgery.
- Pain that worsens with certain movements or physical activities.
- In some cases, numbness or tingling in the pelvic region.
Management: Post-surgical pelvic pain is typically managed with pain relief medications, physical therapy, and in some cases, interventions to address scar tissue or nerve issues.
Conclusion
Pelvic pain is a broad and multifaceted issue that affects both men and women. Whether the pain is anterior, posterior, or associated with pelvic floor dysfunction, identifying the underlying causes and symptoms is essential for effective management.
Various specific conditions such as pregnancy-related pain, athletic pubalgia, and postpartum issues contribute to pelvic discomfort, while gender-specific issues further complicate diagnosis and treatment.
By understanding the different types and causes of pelvic pain, individuals can take proactive steps toward diagnosis, treatment, and recovery. Approaches such as physical therapy, lifestyle modifications, medical interventions, and support from healthcare professionals are vital to improving quality of life for those living with pelvic pain.
