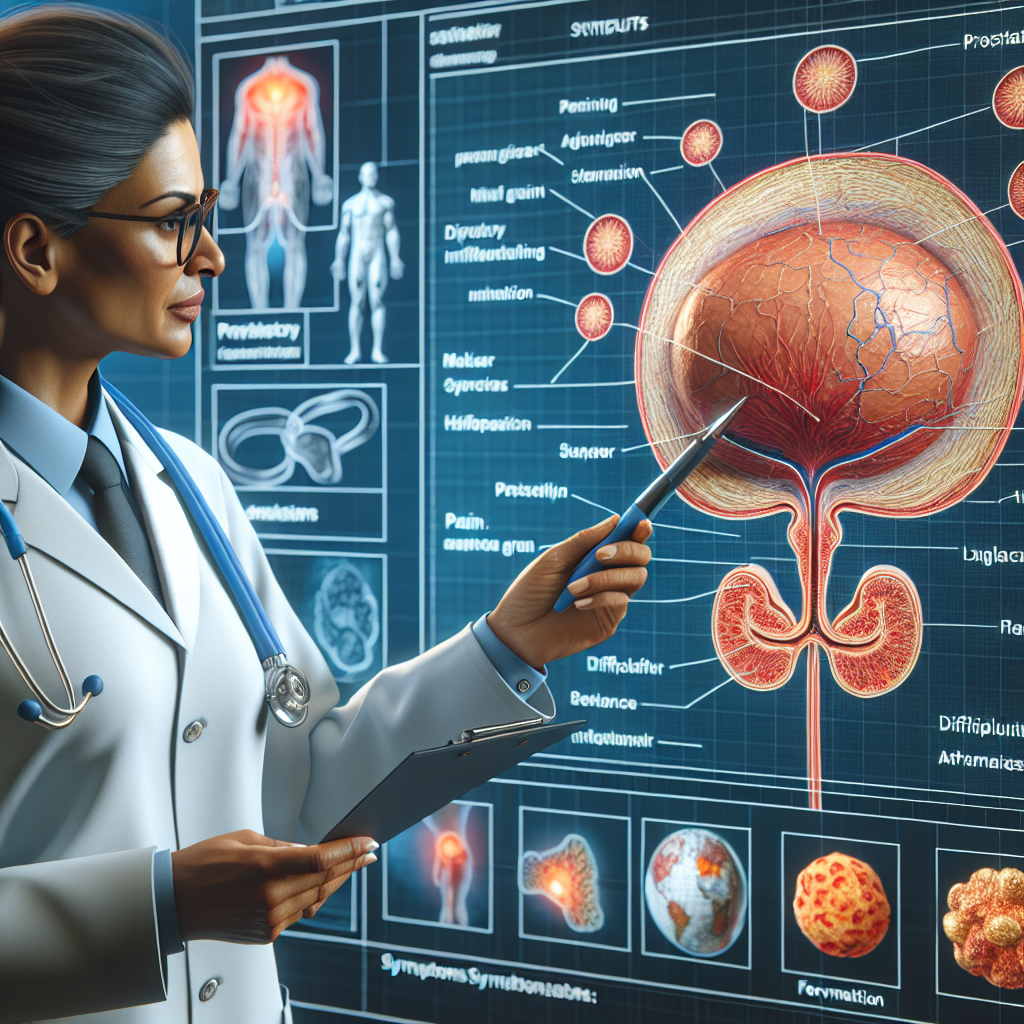
Prostatitis is a condition that extends beyond the prostate gland alone.
For a physiotherapist, it is important to understand how Prostatitis can affect the musculoskeletal system, particularly the pelvic floor, and how targeted interventions can help alleviate symptoms.
As a specialist working with this condition, one must have a comprehensive understanding of the anatomy, common causes, symptom presentation, and specialized tests related to Prostatitis from a physiotherapeutic perspective. This knowledge forms the foundation for effective assessment and treatment.
What Is Prostatitis?
Prostatitis is an inflammation of the prostate gland that can lead to chronic pelvic pain, urinary difficulties, and discomfort in surrounding areas. From a physiotherapy standpoint, Prostatitis is not only seen as a glandular issue but also as a condition with significant musculoskeletal implications. The inflammation can affect pelvic floor muscles, leading to muscle tension, spasms, and referred pain in adjacent areas such as the lower back, hips, and perineum.
Understanding Prostatitis involves recognizing the interaction between the prostate gland and the pelvic floor. A physiotherapist focuses on how changes in muscle tone, posture, and movement patterns can contribute to or result from this condition. This holistic approach considers the body as an interconnected system, where addressing musculoskeletal factors can play a critical role in managing and alleviating symptoms.
Anatomy of the Prostatitis
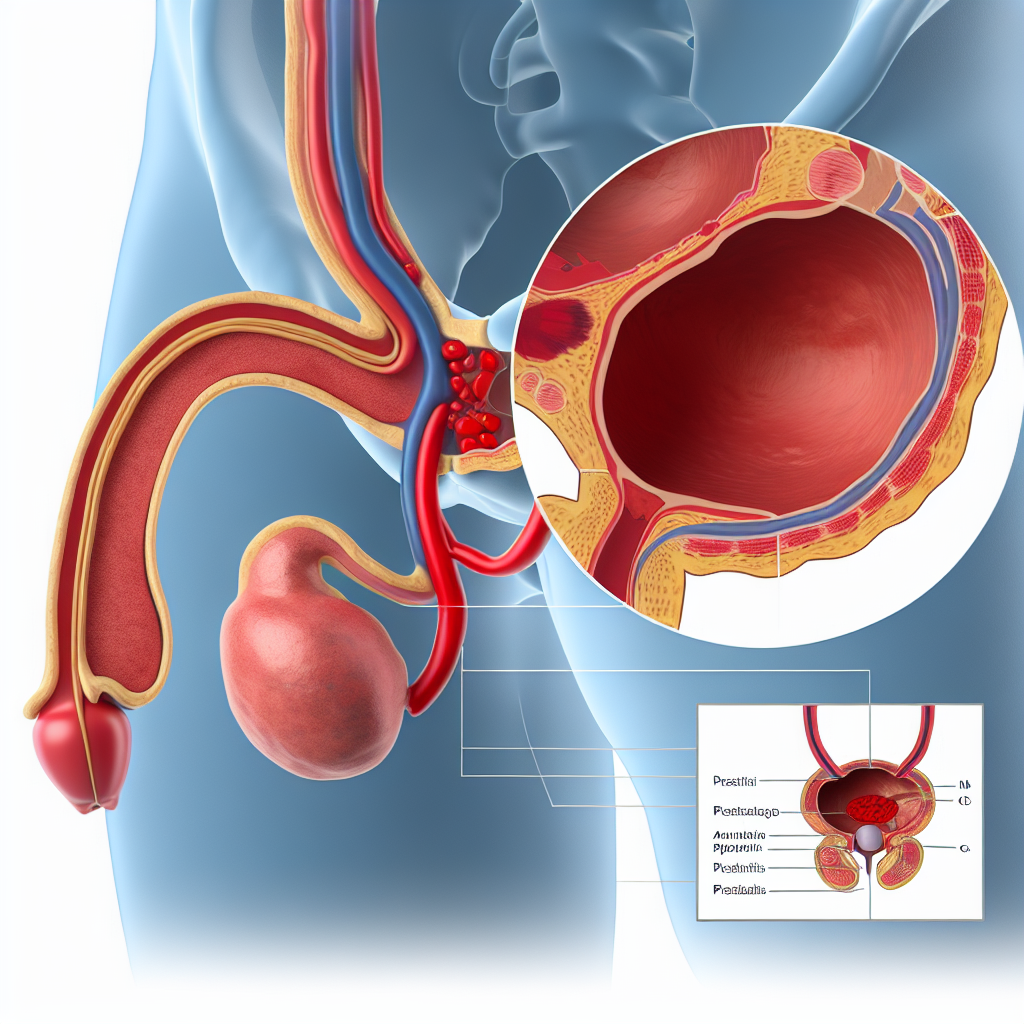
Structure and Location of the Prostate
The prostate gland is situated below the bladder, surrounding the urethra, and anterior to the rectum. Although the gland itself is the primary site of Prostatitis, its location in the pelvic region means that any inflammation can have widespread effects on nearby structures. Physiotherapists must be familiar with this anatomy to understand how Prostatitis interacts with the musculoskeletal system.
Pelvic Floor and Surrounding Muscles
The pelvic floor muscles support the prostate and other pelvic organs. They control bladder and bowel functions and contribute to sexual health. In Prostatitis, these muscles often become tense, spastic, or dysfunctional, which can exacerbate pain and urinary symptoms. Physiotherapists are trained to assess and treat dysfunction in these muscles, which is crucial in managing the condition.
Key pelvic muscles and structures include:
- Pubococcygeus Muscle: Often tense in cases of pelvic pain, contributing to urinary and sexual dysfunction.
- Bulbocavernosus Muscle: Involved in ejaculation and pelvic floor stability, which may become strained.
- Levator Ani Group: Supports pelvic organs and can be a source of referred pain if tight.
Nerve Connections and Referred Pain Patterns
The prostate is innervated by branches of the pelvic and pudendal nerves. These nerves also supply nearby muscles and skin, leading to complex pain referral patterns. A physiotherapist must recognize these patterns to identify whether pain originates from the prostate, pelvic floor muscles, or other structures. Effective treatment often requires addressing nerve entrapment or irritation through manual therapy and neuromuscular re-education techniques.
What Causes Prostatitis?
While the exact causes of Prostatitis can be multifactorial, physiotherapists often concentrate on the mechanical and functional aspects that contribute to the condition.
Musculoskeletal Contributions
- Pelvic Floor Dysfunction: Chronic tension and spasm in the pelvic floor muscles can cause inflammation in the prostate. Prolonged contraction or improper coordination of these muscles may increase pressure on the prostate and surrounding tissues.
- Postural Issues: Poor posture, especially prolonged sitting, can place undue pressure on the pelvic region. This pressure may lead to muscle imbalances and contribute to inflammation.
- Trauma or Injury: Previous injuries to the pelvic or lower back region can alter muscle function, leading to compensatory patterns that affect the prostate.
Psychosocial and Lifestyle Factors
- Stress and Anxiety: High levels of stress can lead to increased muscle tension, particularly in the pelvic floor. Physiotherapists observe that stress management is a vital component of treatment.
- Sedentary Lifestyle: Lack of movement can lead to stiffness, reduced circulation, and muscle weakness, all of which can contribute to the development or exacerbation of Prostatitis.
Interaction with Other Conditions
Physiotherapists understand that Prostatitis can coexist with or mimic other musculoskeletal conditions such as myofascial pain syndrome, pelvic floor dysfunction, or chronic lower back pain. They consider these interactions when assessing the patient to ensure a comprehensive treatment approach.
What are the Symptoms of Prostatitis?
Physiotherapists often encounter patients presenting with a cluster of symptoms that have a musculoskeletal component. Recognizing these symptoms allows for targeted interventions.
Common Musculoskeletal Symptoms
- Pelvic Pain: This can be a deep, aching pain localized around the prostate, perineum, and surrounding muscles. It may radiate to the lower back, hips, or thighs.
- Muscle Tension and Spasms: Increased tone in the pelvic floor muscles, buttocks, lower abdominal, and sometimes the lower back muscles.
- Pain During Movement: Certain postures or activities, like prolonged sitting, walking, or squatting, can exacerbate pain due to muscle strain or nerve impingement.
- Referred Pain: Pain originating from the prostate or pelvic floor may be felt in distant areas such as the lower back, hips, or legs.
Urinary and Sexual Symptoms (Physiotherapist Awareness)
While the primary focus may be on musculoskeletal factors, physiotherapists also need to be aware of how Prostatitis can affect urinary and sexual function:
- Urinary Frequency and Urgency: Patients may feel the need to urinate more frequently or experience urgency due to pelvic floor muscle tension.
- Painful Ejaculation: Discomfort during or after ejaculation, which may be linked to muscle spasms or poor coordination.
- Difficulty with Urine Flow: Muscle tension may contribute to a sense of incomplete bladder emptying or weak stream, related to pelvic floor dysfunction.
Understanding these symptoms helps the physiotherapist develop a holistic treatment plan that addresses both the physical and functional aspects of Prostatitis.
Special Test of Prostatitis
Special tests from a physiotherapist’s perspective focus on assessing the pelvic floor and related musculoskeletal structures. These tests help identify muscle dysfunction, trigger points, and biomechanical issues that contribute to Prostatitis symptoms. Below are key assessments and how they are performed.
Pelvic Floor Muscle Palpation
Physiotherapists trained in pelvic health often perform internal and external palpation of the pelvic floor muscles. This evaluation helps determine:
- Muscle Tone: Identifying hypertonicity or hypotonicity in the pelvic floor.
- Trigger Points: Locating areas of tenderness or knots in the muscles that may refer pain to the prostate region.
- Coordination and Relaxation Ability: Assessing how well the patient can contract and relax pelvic muscles.
How to Perform:
- Preparation: The patient is positioned comfortably, often in a side-lying or supine position with knees bent to relax the pelvic region.
- External Palpation: The therapist begins with gentle palpation of the perineum and lower abdomen to assess muscle tension and tenderness.
- Internal Palpation (if indicated and consented): Using gloved fingers, the therapist carefully inserts a finger into the rectum to feel the pelvic floor muscles surrounding the prostate.
- Assessment: The therapist asks the patient to contract and relax the muscles, noting any asymmetry, pain, or inability to isolate contractions.
Movement and Postural Assessment
Poor posture and movement patterns can contribute to Prostatitis symptoms. A physiotherapist conducts a thorough assessment of:
- Sitting Posture: Evaluating how prolonged sitting may affect pelvic floor tension.
- Gait Analysis: Observing walking patterns to identify compensatory movements that might strain the pelvic area.
- Functional Movements: Assessing movements such as squatting, bending, and lifting to see if they aggravate symptoms or reveal muscle imbalances.
How to Perform:
- Observation: The therapist observes the patient’s natural posture and movements, noting areas of tension or poor alignment.
- Functional Tests: The patient may be asked to perform specific tasks or exercises while the therapist observes for signs of muscle guarding, imbalance, or pain.
- Analysis: The therapist links postural or movement dysfunctions to potential sources of Prostatitis-related discomfort, guiding targeted treatment interventions.
Nerve and Soft Tissue Assessment
Since Prostatitis symptoms can be related to nerve entrapment or soft tissue restrictions, physiotherapists may perform tests to evaluate these aspects.
- Neuromuscular Testing: Testing sensitivity along nerve pathways that innervate the pelvic region, such as the pudendal nerve, to identify areas of hyperirritability.
- Soft Tissue Mobilization Assessment: Checking for restrictions or adhesions in the fascia, muscles, and connective tissues around the pelvis that might be contributing to pain.
How to Perform:
- Palpation for Tenderness: The therapist palpates along the course of relevant nerves and soft tissue structures to locate areas of sensitivity or tightness.
- Provocative Tests: Applying light pressure or stretching specific tissues to see if symptoms are reproduced, which can indicate involvement of certain muscles or neural pathways.
- Integration with Other Findings: Results from these tests are combined with pelvic floor and movement assessments to create a full picture of how the musculoskeletal system is affecting Prostatitis.
Special Pelvic Floor Assessments
Physiotherapists also use biofeedback and manual techniques to gauge muscle function more quantitatively.
- Biofeedback Tools: These devices measure muscle activity to help patients learn to relax or contract muscles correctly, offering visual or auditory feedback.
- Manual Trigger Point Release: Identifying and releasing trigger points in pelvic floor muscles to reduce referred pain and muscle tension.
How to Perform:
- Biofeedback Setup: Electrodes or sensors are placed on or near the pelvic floor muscles. The patient performs contractions or relaxations while the device monitors muscle activity.
- Manual Techniques: Using hands-on techniques to apply pressure to identified trigger points, the therapist works to release tension and improve blood flow.
- Reassessment: After interventions, the therapist reassesses muscle tone and function to gauge improvement and adjust the treatment plan.
How do we Treat Prostatitis
Treating Prostatitis from a physiotherapy perspective involves a multifaceted approach tailored to the patient’s unique musculoskeletal profile. The goal is to reduce pain, improve pelvic function, and empower patients with self-management strategies.
Once a thorough assessment is complete and the musculoskeletal contributors have been identified, the physiotherapist can devise a plan that typically involves a combination of manual therapy, exercise, education, and lifestyle modifications.
Prostatitis Treatment Approaches
Manual Therapy and Soft Tissue Techniques
Manual therapy is a cornerstone in treating Prostatitis, focusing on releasing muscle tension in the pelvic floor and surrounding areas. Techniques include:
- Myofascial Release: Gentle sustained pressure to release restrictions in the fascia around the pelvic area.
- Trigger Point Therapy: Targeted pressure on hyperirritable spots within muscles to relieve referred pain.
- Joint Mobilization: If pelvic joints or the lower back exhibit stiffness, gentle mobilization may help restore movement and reduce strain on pelvic tissues.
Pelvic Floor Muscle Retraining
An essential part of therapy, retraining aims to restore proper muscle balance and function. This often involves:
- Relaxation Techniques: Teaching patients how to consciously relax pelvic floor muscles, using breathing exercises and biofeedback.
- Strengthening Exercises: When appropriate, targeted exercises to strengthen weak pelvic floor muscles without causing tension, often using techniques like Kegels under guidance.
- Coordination and Control Training: Helping patients learn to coordinate muscle contractions and relaxations, improving bladder and bowel function and reducing pain.
Postural Re-education and Movement Correction
Correcting posture and movement patterns can alleviate undue pressure on the prostate and pelvic floor. Treatment strategies include:
- Ergonomic Advice: Adjusting seating, workstations, and daily habits to reduce pelvic strain.
- Core Stability Training: Enhancing core strength to support the pelvis and reduce compensatory muscle tension.
- Stretching and Flexibility Exercises: Targeting hip flexors, lower back, and leg muscles to release tension that may affect pelvic alignment.
Education and Self-Management Strategies
Empowering patients with knowledge and tools is a key component of physiotherapy care:
- Postural Awareness: Teaching patients how to maintain proper posture during daily activities to minimize pelvic strain.
- Stress Management: Providing guidance on relaxation techniques, mindfulness, and stress reduction to ease pelvic muscle tension.
- Lifestyle Modifications: Recommendations for avoiding prolonged sitting, integrating regular movement breaks, and modifying activities that trigger symptoms.
Prostatitis Differential Diagnosis
From a physiotherapist’s perspective, differential diagnosis focuses on distinguishing Prostatitis-related musculoskeletal issues from other conditions with similar presentations. This includes:
- Pelvic Floor Myofascial Pain Syndrome: Overlap in symptoms like pelvic pain and muscle tightness; treatment strategies may be similar but guided by precise assessment.
- Lower Back Pain Syndromes: Differentiating referred pain from lumbar spine issues versus pain originating in the pelvic region.
- Urinary Dysfunction without Prostatitis: Ensuring that urinary symptoms are linked to musculoskeletal dysfunction rather than solely urological issues.
- Abdominal or Hip Pathologies: Rule out hip joint issues, abdominal muscle strain, or nerve entrapments that may mimic Prostatitis symptoms.
Physiotherapists use their specialized training in musculoskeletal assessment to distinguish these conditions, often working in collaboration with other healthcare professionals for comprehensive care.
Prostatitis Prognosis and Expectations
While Prostatitis can be a chronic and challenging condition, physiotherapy often leads to significant improvements in pain management and function. Setting realistic expectations involves:
- Gradual Improvement: Patients may notice slow but steady improvement in muscle tension, pain levels, and urinary function over weeks or months of regular therapy.
- Self-Management Skills: Patients learn techniques to manage flare-ups, reduce muscle tension, and prevent recurrence, leading to longer-term improvements.
- Multidisciplinary Collaboration: Successful management often involves working with medical doctors, urologists, and mental health professionals, with physiotherapy serving as a key component in the team approach.
Physiotherapists communicate that while complete resolution may not occur immediately, ongoing therapy and adherence to exercise and lifestyle recommendations typically yield a better quality of life, reduced pain, and improved pelvic function.